How General Practice Works
We know that patients are constantly hearing the NHS is under pressure, whether it is news stories about waiting lists, patient satisfaction, or what you are told when accessing services.
We also know how frustrating that can be when all you are trying to do is get help with your health.
We wanted to give some background about where these challenges come from and how changes you might see are designed to help patients and practices work as well as we can.
But before we go any further, please know this: Your health is our number 1 priority, and we want you to continue to come forward for care when you are unwell.
This article is not intended to put people off using the NHS or to make anyone feel guilty. It’s about giving some broader context to the circumstances we’re operating in.
With that said, scroll down to read more, watch the video below or use the buttons to jump to specific sections.
About the NHS
Let’s start with a nice simple fact: The NHS is enormous.
The NHS directly employs 1.7 million people, making it the fifth biggest employer in the world.
For context, the NHS sits behind the Indian and US defence services, the Chinese army and Walmart. Amazon is in 6th place behind the NHS.
The NHS budget for 2023/24 is £187 billion.
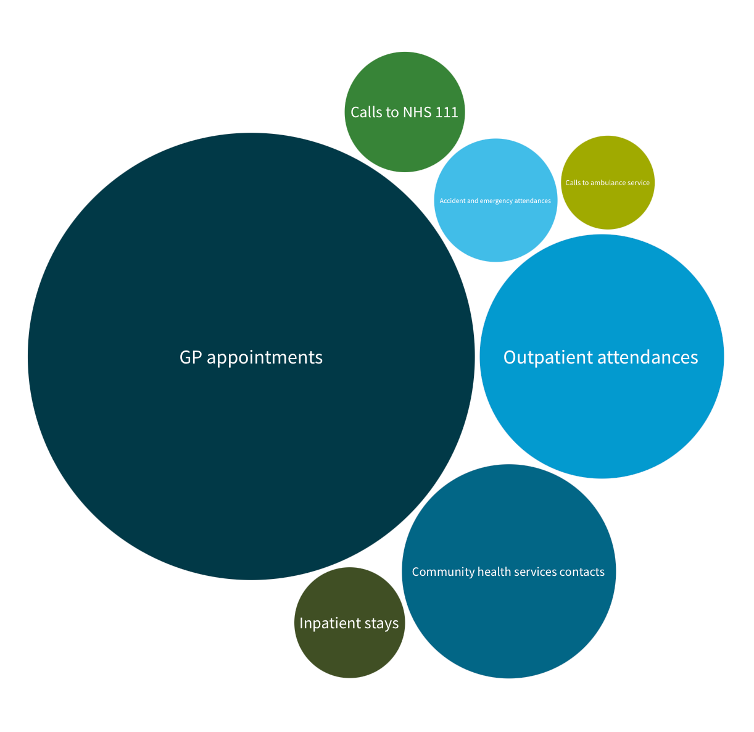
Figures from the King’s Fund in 2023 showed that the NHS had more than 1.6 million contacts with patients daily.
This includes all hospital stays and outpatient appointments, community, ambulance, and mental health services, but the bulk is delivered in General Practice.
The share of the NHS budget that goes to GP practices to deliver these appointments is 8.4%.
About General Practice
Funding for each GP practice comes via what are called Integrated Care Boards. These 42 regional NHS organisations commission services for patients in their area.
GP practices are then contracted to provide core services, with a set amount of money per patient.
The core services include:
- Care and treatment
- Referrals to specialists
- Managing long-term conditions
- Promoting health
- Out-of-hours provision
- Preventative health measures like cervical screening, vaccinations and immunisations.
Each practice receives £164 yearly to look after each patient. That works out to 66p per patient for every day we are open.
Why the NHS is stretched
If you read or listen to news stories about the NHS, you might frequently hear the words ‘demand’ and ‘capacity’.
Demand is the needs of patients, and capacity is our available resources.
When demand is higher than capacity, waiting times get longer.
Some figures comparing the NHS in 2015 and 2024 help illustrate this.
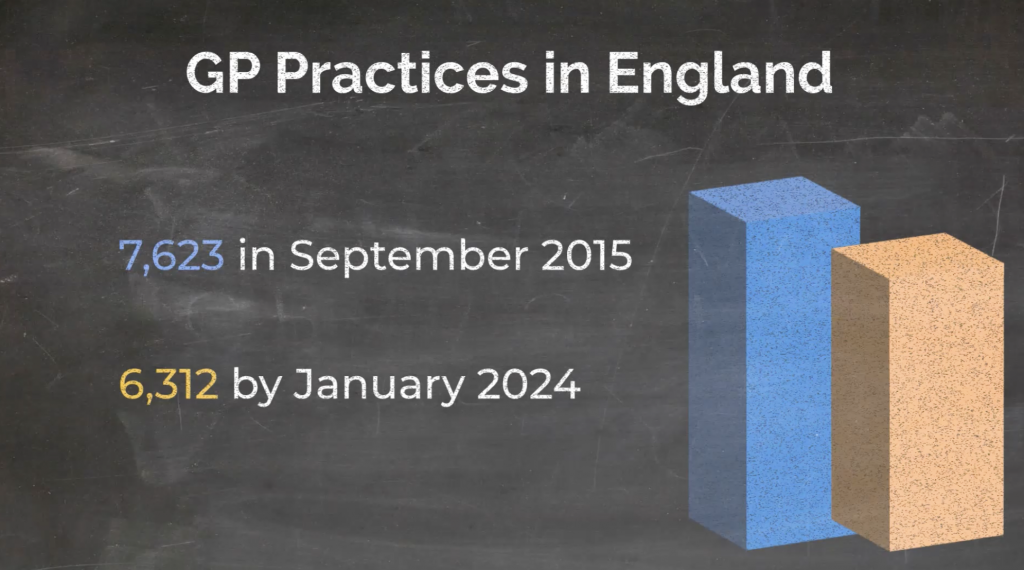
In September 2015, there were 7,623 GP practices in England. By January of this year, that number was 6,312. So, we have lost 1,300 GP practices in over eight years.
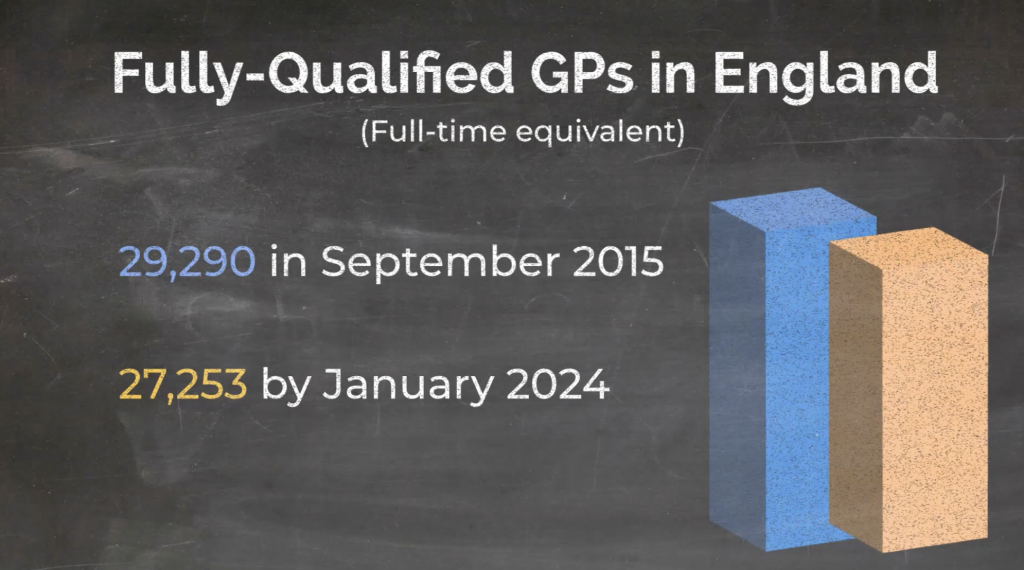
At the same time, figures from the BMA show that the number of fully qualified GPs has dropped from 29,290 to 27,252. This is based on full-time equivalent roles, and the same statistics show a shift in more Doctors working fewer hours to protect their work-life balance.
So, there are fewer GP practices and fewer GPs. What about patient numbers?
That has increased by over 6 million.
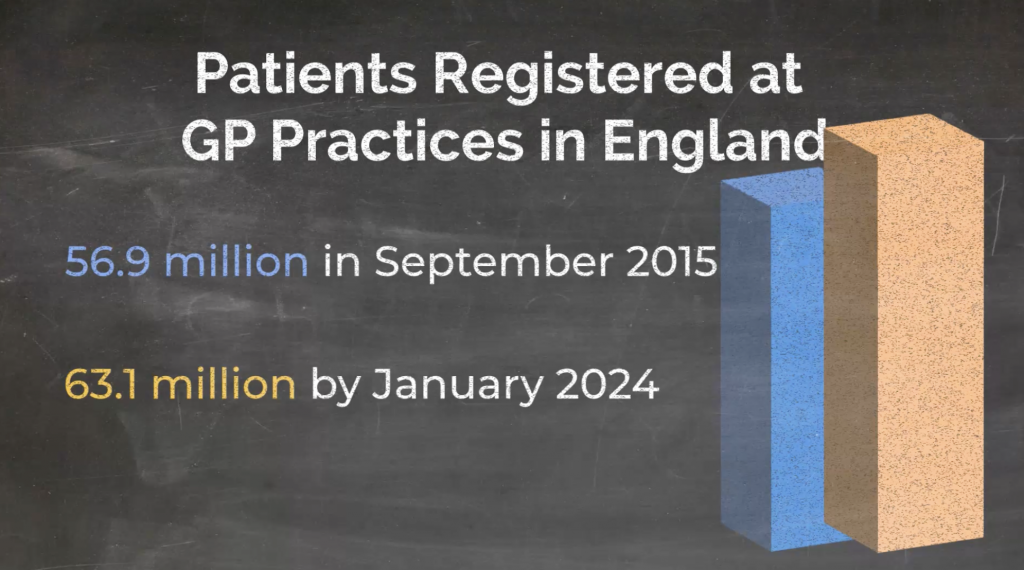
In January this year, 63.1 million people were registered with GP practices in England. That’s up from 56.9 million in September 2015.
What that means for practices is that, on average, they have 2,500 more patients, with each GP responsible for an additional 357 people.
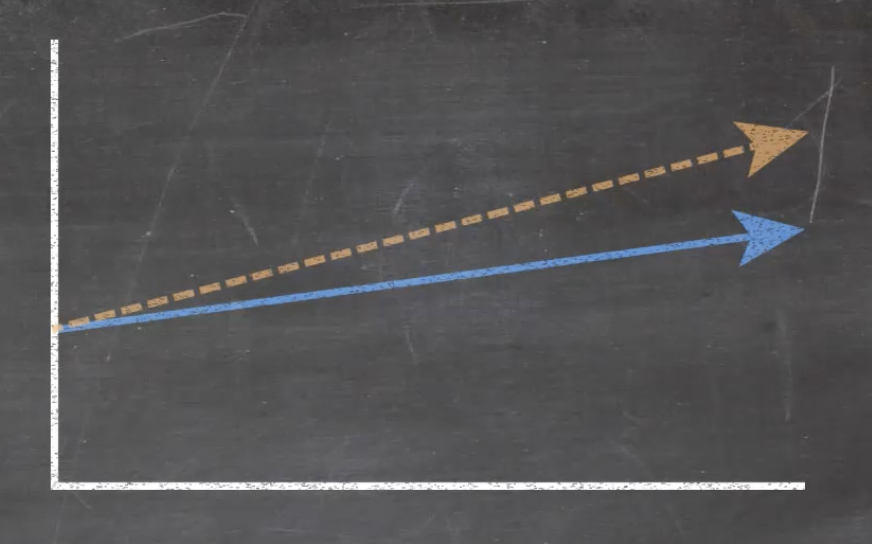
Your next question might be if the NHS budget has grown as well. The answer is yes and no.
Yes, the NHS budget goes up every year. But in the ten years before the pandemic, it increased slower than before. Had it continued at the same rate, there would have been an additional £322 billion in the budget.
Inflation and the cost of living are also relevant here. As the cost of running GP practices – everything from sticky plasters to gas and electricity – increases, our budgets don’t go as far as they used to.
Not only are practices dealing with significantly bigger populations, but we are an ageing population with increased needs.
Life expectancy has increased by over four years since the start of the century. And the number of people with long-term health conditions like diabetes, asthma, COPD, high blood pressure, or mental health issues has also gone up.
Just eight years ago, the number of people who needed ongoing management for incurable conditions was 29%. Now it is 36%.
This all adds up to more than 1 million people being seen in General Practice daily. Taken over a year, it’s nearly 360 million appointments. That’s more than 5 per person every year.
Meeting Patients needs
The NHS is changing to meet patients’ needs, and GP practices are no exception.
We have to find ways to meet patients’ needs with the resources that we have. We’d love to be able to offer a same-day, face-to-face appointment for everyone who wants one or a quick and efficient referral to another service that solves an issue, but that just isn’t always possible.
Here are some ways we’re adapting and how they help.
The increased use of digital technologies like the NHS App and online consultations benefits patients and practices.
Every prescription ordered or test result checked on the NHS App or issue resolved via an online consultation makes it easier to see you in person when needed.
Many online options are also considerably quicker than making a phone call or visiting the practice, and others are also available outside of our regular opening hours.
Sometimes, you might also be offered an appointment with someone other than a Doctor, such as an Advanced Practitioner.
Their additional training means they can assess and treat a wide range of conditions and prescribe medicine or arrange further care. Often, you will be able to get a resolution quicker than waiting to see a GP.


Local pharmacies can also treat and prescribe medication for seven common conditions like earache, skin infections, and urinary tract infections. You don’t need to be referred or see a GP first. You can walk into any pharmacy without an appointment; some are open in the evenings and weekends, too.
Then there are our Primary Care Networks (PCN) – where groups of GP practices work together to provide additional expert services.
You can read more about our PCN teams’ work in Gosforth and Jesmond. The thousands of medication reviews, home visits, same-day appointments, long-term condition reviews, and Social Prescribing appointments are all part of an extra level of services to meet patients’ needs.
What patients can do
As we said at the top, this isn’t intended to dissuade you from using NHS services when you need them.
The NHS was set up to serve the people who need it. Free at the point of use and based on your clinical need.
This article aims to share some of the background to the challenges we face and go a bit deeper than the headlines you might see.
It’s also to hopefully reassure you that there is a logic behind options you might be offered, even if they are unfamiliar or not what you were expecting.
When Reception or Admin staff ask about your issue, it’s because they’re trained to know the best way to help you.
Or if we suggest using the NHS App for your prescriptions, it’s not to get you off the phone; it’s to save you time and effort and allow us to help more patients.
If an advanced practitioner sees you, it’s because they can treat and manage your condition just as well as a GP, and they’re available sooner.
We know getting the help you need when you’re unwell can be stressful, and we understand patients’ frustration. Please know that we share those frustrations and are committed to getting you the best possible care.